In the final draft of the UN non-communicable disease (NCD) declaration, obesity was omitted. That indicates there is more work to be done.
At a recent Economist Impact event about obesity, sponsored by Novo Nordisk, on the sidelines of the UN General Assembly, one message came through clearly: tackling obesity will depend on embedding it firmly into the global NCD response. Without doing so, many will get left behind.
“We need to hardwire obesity into the NCD agenda”
Jagat Narula, President, World Heart Federation
Calls to action:
1
Advocating for obesity as an NCD
Enhancing co-operative advocacy efforts across the NCD community around obesity as a disease that needs a stronger health system response to prevention and management.
2
Lead with science
Incentivising obesity action as an economic, social and health “best buy”. Create a data lifecycle that uses existing data to inform policy, then uses data from implementation to further build an evidence base showing broad fiscal and health returns upon which to build future policy interventions.
3
Put people with lived experience at the centre
People with lived experiences should have a core voice in the process of designing obesity prevention and management policies.

As Jagat Narula, President of the World Heart Federation pointed out: “We won’t hit Sustainable Development Goal 3.4 without slowing obesity trends.” Doing so will require a multi-pronged approach—combining stronger prevention, treatment and governance within a unified whole of society response. As highlighted in our National Obesity Action Plan Playbook, success depends on embedding obesity into broader health and development strategies, backed by clear goals and shared accountability. It is and will be a test of commitment and political will.
The question, then, is how we ensure that the global momentum and conversations on obesity are turned into national and local action? How do we guarantee that obesity is not yet again left out of the policy agenda and ensure change for people living with obesity?
From disappointment to determination
For many advocates, this has been a familiar struggle. Progress has been slow, recognition uneven, and optimism tested. Charline Coquerel Couniot, Vice president of patient experience and advocacy at Novo Nordisk cautioned against dwelling on this sentiment: “We shouldn’t dwell on the disappointment,” she said. “Obesity is a disease, and we must continue to say it, even when official documents don’t.”
That determination carries a strong conviction that will be the driving force for change. Continued advocacy will not only shift perceptions, but demand policy change. And when policy moves, so do the systems and recognition surrounding obesity.
“Obesity is a disease, and we must continue to say it, even when official documents don’t.”
Charline Coquerel Couniot, Vice president of patient experience and advocacy, Novo Nordisk
“Obesity is really what connects NCDs. And you really need to think about how to tackle obesity in a holistic way if you really want to have impact in many other NCDs.”
Dr Simón Barquera, Director of the Nutrition and Health Research Centre at the National Institute of Public Health, Mexico
To tackle obesity—and therefore NCDs—effectively, we need to change how we perceive obesity, and how we manage it in a way that acknowledges what we know about the science of obesity. First, obesity must be recognised as a disease in its own right, and as a strategic entry point for broader NCD prevention, care and policymaking. Second, addressing it requires an integrated, coordinated approach of policymaking and of care that spans across specialties, systems and stages of life. A failure to do both will not prepare us well for the serious economic and developmental consequences of this epidemic.
We’ve long known that integrated care is the answer. But knowing is not the same as doing. So where do we start?

Key elements
Unifying collaboration: Addressing obesity demands a whole-of-society approach, detailing and assigning stakeholders’ responsibilities across government, academia, NGOs and the private sector to ensure accountability, efficiency and impact.
Integrating policy approaches: A “health-in-all-policies” approach embeds health considerations into policies across sectors, such as urban planning, education, and agriculture. This is essential to tackle the underlying social and environmental drivers of obesity, while also ensuring people living with obesity have access to quality care they need.
An economy-first argument
Continuous articulation that obesity is not only a health challenge, but an economic and development issue, is important to turn recognition of obesity into policy action. Dr Narula argued that the next phase must move “from health-first to economy-first framing, to show why investment is needed and what returns it will generate.”
Communicating policies on obesity and related NCDs as economic “best buys,” grounded in evidence of both health and fiscal returns, can shift the conversation from cost to opportunity. It may even inspire other countries to follow suit. This was the case for Mexico, as Simón Barquera, Director at the Centre for Research in Nutrition and Health in Mexico’s National Institute of Public Health has observed: “In Mexico, one way to push policies is to demonstrate that they work,” he said. “It took 14 years to pass the soda tax, but once it happened, it inspired many other countries to follow. Policymakers act when they see results—and when they see an opportunity to have a legacy.”
Dr Barquera added that Mexico has reinvested sugar sweetened beverage tax revenues into obesity prevention and management. This direct reinvestment cycle generates funds and trust among the public.
“Policymakers act when they see results—and when they see an opportunity to have a legacy.”
Simón Barquera, Director, centre for research in nutrition and health, Mexico’s National Institute of Public Health

Policy suggestion
Policymakers recognising obesity as a disease is a priority, but it is also important to recognise how obesity impacts development, economic and equity. Framing the prevention and management of obesity in this broader context enables interministerial collaboration across government to address the underlying drivers of the disease.

We need to give people the tools and environment to live healthier for longer. If our surroundings are working against us, even the best intentions of action cannot be realised. This involves looking at other sectors as well. Take urban design: if neighbourhoods are not built with safe pavements, nearby parks or affordable leisure activities, then opportunities for physical activity disappear. We tell people to move, but what if there is nowhere safe or affordable to go?
“Health in all policies is the trigger to make things happen. It is an accelerator. The health sector worked hard for many years; they cannot do it alone.”
Dr. Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
That is why intersectoral policy and planning at the system level matters. People need environments that make healthy choices not just possible, but easier, to live their healthiest lives.
Galvanising public understanding of obesity
Deepening the understanding of the science of obesity remains one of the most powerful tools for achieving obesity policy prioritisation and improving people living with obesity’s experiences of interacting with the health service. During the discussion, audience members called for lifelong public education on nutrition and health; not only in schools, but across communities, workplaces and health systems. Teaching people to read food labels, supporting peer-led coaching, and embedding obesity awareness, education and literacy into curricula were seen as galvanising mechanisms for change.
“Knowing is not enough; we must apply. Willing is not enough; we must do.”
Jagat Narula, World Heart Federation
Writing our own next chapter in obesity prevention and management
Education should also extend to reducing the stigma associated with obesity, by proactively promoting the science of obesity and correcting misconceptions across society. This includes initial medical training and continuing medical education.
Ultimately, education should go beyond awareness and help build advocacy from citizens to policymakers. Changing how societies think about obesity, pivoting to seeing it as a disease with complex biological, social and environmental causes, rather than an individual failure, will enable the general public to understand why policy action is needed and why particular approaches—from taxation to management—are needed.
“Obesity is a long-term trend; you don’t have success in minutes, or even in years. You need at least 10 years of sustainability to see significant changes.”
Martine Laville, Professor Emeritus, Lyon 1 University, France
Imagine Jason again.
But this time, he lives in a world where obesity is taken seriously as a disease. As a result, its prevention and management is integrated into every day health promotion and health care services. He is included actively in his care plan, knows where to go and who to turn to. His care is connected between services and not scattered across them, and most potential complications are caught before they escalate. Jason no longer feels confused or blamed by the system. Instead, he feels supported, seen and in control of his health.
That is the kind of health care system people living with obesity deserve. And integrating obesity prevention and management into NCD care is one major step in that direction.


Key elements
Unifying collaboration: Addressing obesity demands a whole-of-society approach, detailing and assigning stakeholders’ responsibilities across government, academia, NGOs and the private sector to ensure accountability, efficiency and impact.
Integrating policy approaches: A “health-in-all-policies” approach embeds health considerations into policies across sectors, such as urban planning, education, and agriculture. This is essential to tackle the underlying social and environmental drivers of obesity, while also ensuring people living with obesity have access to quality care they need.
Putting lived experiences at the centre
“Incorporating lived experience is not ‘nice-to-have’—it’s central.”
Amber Huett-Garcia, lived-experience advocate
Among the messaging and education, the most important is that the realities of those living with obesity are heard. Amber Huett-Garcia, lived-experience advocate, emphasised that this “Is not ‘nice-to-have’—it’s central.”
Involving people with lived experience, she elaborated, changes how policymakers understand, and shape the issue. “We need to educate them on what obesity really is—on the science, on stigma and on why seeing obesity as a disease benefits other NCD responses too,” she said. When those most affected shape the discussion, systems become more informed, tailored and equitable.
Amber also reiterated the importance of citizen advocacy: “People change policy,” she said. “If you’re not satisfied, call your policymaker–and call a friend to call theirs.” Building such momentum is vital to build political will that translates into action by citizens holding political representatives to account.

Policy suggestion
Policymakers recognising obesity as a disease is a priority, but it is also important to recognise how obesity impacts development, economic and equity. Framing the prevention and management of obesity in this broader context enables interministerial collaboration across government to address the underlying drivers of the disease.

We need to give people the tools and environment to live healthier for longer. If our surroundings are working against us, even the best intentions of action cannot be realised. This involves looking at other sectors as well. Take urban design: if neighbourhoods are not built with safe pavements, nearby parks or affordable leisure activities, then opportunities for physical activity disappear. We tell people to move, but what if there is nowhere safe or affordable to go?
“Health in all policies is the trigger to make things happen. It is an accelerator. The health sector worked hard for many years; they cannot do it alone.”
Dr. Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
That is why intersectoral policy and planning at the system level matters. People need environments that make healthy choices not just possible, but easier, to live their healthiest lives.
Key elements
Unifying collaboration: Addressing obesity demands a whole-of-society approach, detailing and assigning stakeholders’ responsibilities across government, academia, NGOs and the private sector to ensure accountability, efficiency and impact.
Integrating policy approaches: A “health-in-all-policies” approach embeds health considerations into policies across sectors, such as urban planning, education, and agriculture. This is essential to tackle the underlying social and environmental drivers of obesity, while also ensuring people living with obesity have access to quality care they need.
Putting lived experiences at the centre
“Incorporating lived experience is not ‘nice-to-have’—it’s central.”
Amber Huett-Garcia, Emeritus Director, Obesity Action Coalition
Among the messaging and education, the most important is that the realities of those living with obesity are heard. Amber Huett-Garcia, lived-experience advocate and Emeritus Director of the Obesity Action Colation, emphasised that this “Is not ‘nice-to-have’–it’s central.”
Involving people with lived experience, she elaborated, changes how policymakers understand and shape obesity prevention and management. “We need to educate them on what obesity really is—on the science, on stigma and on managing obesity as a disease benefits other NCD responses too,” she said. When those most affected by obesity shape the discussion, systems become more informed, tailored and equitable.
Ms Huett-Garcia also reiterated the importance of citizen advocacy: “People change policy,” she said. “If you’re not satisfied, call your policymaker–and call a friend to call theirs.” Building such momentum is vital to build political will that translates into action by citizens holding political representatives to account.



“Health in all policies is the trigger to make things happen. It is an accelerator. The health sector worked hard for many years; they cannot do it alone.”
Dr. Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
That is why intersectoral policy and planning at the system level matters. People need environments that make healthy choices not just possible, but easier, to live their healthiest lives.
Beyond the declaration and keeping momentum
Despite obesity’s omission from the final draft UN NCD declaration, there’s hope for the next high level meeting. Experts agreed that the path forward is clear. Dr Barquera said, “We know what we have to do. We have the evidence and the best buys.” This was echoed by Ms Huett-Garcia: “We can do things, we just aren’t.”
UNGA was one, but far from the only moment to get obesity on the broader health, political, economic and social agenda. Critical next steps will include identifying opportunities and mechanisms for getting obesity recognised and managed as an NCD and integrating it into the NCD agenda. Embracing an all of society approach to incorporate a broad range of stakeholders is one way, enhanced by proactively taking the conversation to them. Also identifying key policymaking moments where obesity policymakers and advocates can raise the profile of obesity, whether that be engaging financial leaders at Davos,broad health stakeholders at the World Health Assembly, or the Universal Health Coverage High Level Meeting in 2027.
“We can do things, we just aren’t.”
Amber Huett-Garcia
As our post on the systems around obesity has shown, the system is not broken beyond repair. It simply needs to be rewired. Hardwiring obesity into the NCD agenda is not the end goal; it is where real change begins.
Recognising the experts
Simón Barquera, Director, centre for research in nutrition and health, Mexico’s National Institute of Public Health (INSP)
Charline Coquerel Couniot, Vice president of patient experience and advocacy, Novo Nordisk
Amber Huett-Garcia, Emeritus Director, Obesity Action Coalition
Jagat Narula, President, World Heart Federation






Audience key take aways
There is a need for all-of-society action on obesity–the solutions do not just lie in the healthcare system.
Position obesity at the heart of NCD prevention–progress on obesity unlocks progress across other major health targets.
A shift in narrative around health system funding to reflect the investment in keeping populations in good health rather than the cost of treating ill health.
We would like to thank the panellists and audience who took part in the discussion at The economic imperative: policy solutions for tackling non-communicable diseases, an Economist Impact event sponsored by Novo Nordisk on the sidelines of Abu Dhabi Global Health Week.
- Buthaina Abdulla Bin Belaila, Head of non-communicable diseases and mental health, Ministry of Health and Prevention, UAE
- Haleama Al Sabbah, Associate professor, Abu Dhabi University
- Sara Suliman, Clinical lead for obesity, genetics of diabetes and endocrinology, Imperial College London, Abu Dhabi
- Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
- Dan Beety, Senior director, global obesity policy and public affairs, Novo Nordisk
We will be continuing the conversation at upcoming events around the World Health Assembly and UN General Assembly, and welcome policymakers, advocates and changemakers to join us in advancing obesity on the global health agenda.
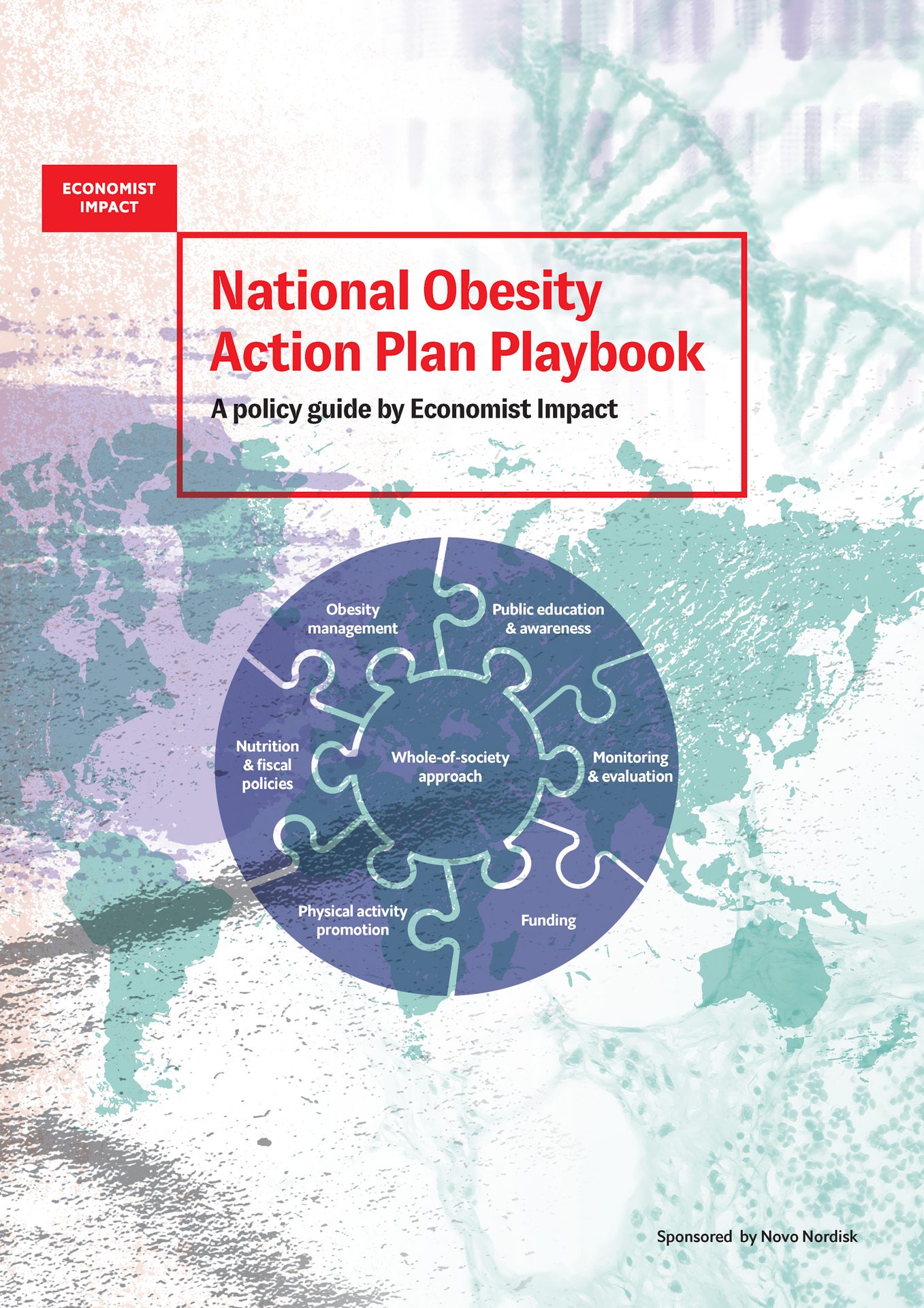
The National Obesity Action Plan Playbook contributes to advancing policy and national action on obesity by providing policymakers with a practical framework for designing and strengthening national strategies to prevent and manage obesity. Drawing on WHO guidance, global expertise, and case studies, it identifies key action areas and highlights best practices for tackling obesity’s systemic drivers through a whole-of-government and whole-of-society approach.
