This year’s global non-communicable disease (NCD) conversation is missing a critical piece. Without urgent action on obesity, the opportunity to meet the targets on tackling NCDs may slip away again.
In September, governments will gather in New York to review progress on non-communicable diseases (NCDs) at the UN General Assembly (UNGA). A new political declaration will follow. But obesity, a disease affecting over one billion people worldwide, is barely mentioned in the draft of the current agenda.
This silence is an oversight that does not recognise that obesity carries serious consequences for health, development and equity. Obesity remains framed as a modifiable risk factor and a matter of lifestyle, addressed mainly through prevention at an individual level rather than systemic change. The science of obesity tells a different story. Obesity is a complex, chronic condition that is the result of an interplay of genetic, biological, psychological, social and environmental factors as recognised by the WHO. Leaving obesity out of the conversation as a disease risks undermining the entire NCD agenda.
“Without action, we're leaving half the world behind - 4 billion people will be affected by overweight and obesity by 2035, with economic costs reaching nearly 3% of global GDP by 2030”
Obesity connects the NCDs we treat in isolation
Imagine a car that is solid, reliable and built to last, but only with regular maintenance–regular oil changes, brake checks, and the occasional new set tyres. Look after it, and it will keep running for years.
This is the metaphor for obesity Dr. Sara Suliman from Imperial College, Abu Dhabi, offered at the recent panel discussion on The economic imperative: policy solutions for tackling non-communicable diseases, an Economist Impact event sponsored by Novo Nordisk on the sidelines of Abu Dhabi Global Health Week.
But unlike machines, human bodies are not all manufactured to identical specifications. Not all cars start from the same blueprint. Some have built-in vulnerabilities–genetic predispositions, early-life exposures, or structural disadvantages–that require more than routine care.
Which is why the metaphor must go one step further. We need to stop fixing parts in isolation and start looking at the whole vehicle and its environment to optimise function. Health systems should be designed with the same mindset: to support the body more holistically, across time and circumstance, integrating care across different disease areas.

Policy suggestion
Recently, The Lancet Global Health published a comment by several leading obesity experts on priority actions for the global obesity response. The first priority action is adopting The World Health Organisation’s (WHO) definition of obesity as a disease, and embedding it in national and global health frameworks, including the UNGA NCD High Level Meeting (HLM) Political Declaration. Doing so would help shift policy focus beyond prevention to include long-term care, while unlocking funding and accountability mechanisms on par with other NCDs.
No progress on NCDs without preventing and managing obesity
“We can't work alone and we can't achieve or tackle obesity or NCDs by one sector. So all of us are responsible for that.”
Professor Haleama Al Sabbah, Associate professor in public health and nutrition at Abu Dhabi University
Obesity is a common thread running through much of the NCD burden. It contributes to type 2 diabetes, cardiovascular disease, musculoskeletal disorders, several cancers and more. Its impacts are economic as well as physical, deepening health inequalities and further straining health budgets.
By 2035, more than half the world’s population is expected to be living with overweight or obesity. Countries that are off track to meet Sustainable Development Goal 3.4 (SDG 3.4)—to reduce premature mortality from NCDs—will fall even further behind unless obesity is prioritised. Tackling obesity unlocks progress across the board.
Yet most policies treat obesity as a risk factor and focus on prevention efforts that are important, but insufficient on their own. There is still limited holistic management for people living with obesity today, or system-level action to prevent and manage the disease. Few health systems are set up to provide the kind of long-term, person-centred support that’s needed. The result is that people living with obesity are left unsupported by health systems and society, and even blamed.

Policy suggestion
National NCD strategies can integrate the prevention and management of obesity. This includes integrating obesity into existing care pathways for other chronic conditions, developing person-centred care pathways, updating clinical guidelines and training providers in holistic obesity management.
“Obesity is really what connects NCDs. And you really need to think about how to tackle obesity in a holistic way if you really want to have impact in many other NCDs.”
Dr Simón Barquera, Director of the Nutrition and Health Research Centre at the National Institute of Public Health, Mexico
To tackle obesity—and therefore NCDs—effectively, we need to change how we perceive obesity, and how we manage it in a way that acknowledges what we know about the science of obesity. First, obesity must be recognised as a disease in its own right, and as a strategic entry point for broader NCD prevention, care and policymaking. Second, addressing it requires an integrated, coordinated approach of policymaking and of care that spans across specialties, systems and stages of life. A failure to do both will not prepare us well for the serious economic and developmental consequences of this epidemic.
We’ve long known that integrated care is the answer. But knowing is not the same as doing. So where do we start?
Key elements
Unifying collaboration: Addressing obesity demands a whole-of-society approach, detailing and assigning stakeholders’ responsibilities across government, academia, NGOs and the private sector to ensure accountability, efficiency and impact.
Integrating policy approaches: A “health-in-all-policies” approach embeds health considerations into policies across sectors, such as urban planning, education, and agriculture. This is essential to tackle the underlying social and environmental drivers of obesity, while also ensuring people living with obesity have access to quality care they need.
Laying a foundation towards a breakthrough
Countries are beginning to recognise obesity as a serious, chronic disease. National strategies are emerging, new models of care and clinical care guidelines are being piloted. Experts describe how some governments have even taken the important step of granting obesity official disease status, which in turn supports the prioritisation and funding of obesity prevention and management. These are early signals of change, and they reflect growing momentum that addressing obesity is an important mechanism in the broader response to NCDs.
The WHO has also outlined a foundation from which momentum can build. Global frameworks such as the WHO Acceleration Plan on Obesity and the WHO Service Delivery Framework provide roadmaps for countries to integrate obesity action across sectors and systems. Our National Obesity Action Plan Playbook highlights the work of several countries that have integrated obesity action across sectors and systems, so that other countries can either build or enhance their own obesity prevention and management plans.
The health, social and economic impacts of obesity make a compelling case for action, but that action is not materialising quickly or extensively enough to hit SDG 3.4 or the WHO’s target to halt the rise in obesity by 2025. The momentum from existing commitments on the ground must be met with political will from the top. Without strong leadership, or a declaration, early progress will stall and the opportunity to scale solutions for people to live healthier for longer will be lost.
“Reducing global rates of obesity and NCDs won’t be about individual willpower—it will be about collective political will to act.”

Policy suggestion
Policymakers recognising obesity as a disease is a priority, but it is also important to recognise how obesity impacts development, economic and equity. Framing the prevention and management of obesity in this broader context enables interministerial collaboration across government to address the underlying drivers of the disease.

We need to give people the tools and environment to live healthier for longer. If our surroundings are working against us, even the best intentions of action cannot be realised. This involves looking at other sectors as well. Take urban design: if neighbourhoods are not built with safe pavements, nearby parks or affordable leisure activities, then opportunities for physical activity disappear. We tell people to move, but what if there is nowhere safe or affordable to go?
“Health in all policies is the trigger to make things happen. It is an accelerator. The health sector worked hard for many years; they cannot do it alone.”
Dr. Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
That is why intersectoral policy and planning at the system level matters. People need environments that make healthy choices not just possible, but easier, to live their healthiest lives.
A call to act now
“We need to take a step back and speak together. Starting with the problem, treating inequities and managing disease at their origin. If we look long term, we save more.”
Dr. Sara Suliman, Imperial College, Abu Dhabi
The current draft declaration falls short. Framing obesity as a risk factor underestimates its potential role in broader NCD prevention and management, and fails to reflect the reality that there are ~1bn people globally living with obesity already in need of support. As it stands, countries may fail to meet the scale and urgency of the challenge ahead.
Policymakers, civil society, the private sector, international institutions must come together to demand better. Obesity should be reinstated as a priority to ensure long-term prevention, so that people living with obesity can receive care for their disease on equal footing with other major NCDs.
Writing our own next chapter in obesity prevention and management
Integrating obesity into national health and development strategies requires political commitment, policy coherence and long-term investment. As countries recommit to frameworks like the WHO Acceleration Plan, they must ensure that obesity policy-making, prevention and management is no longer siloed or treated as an afterthought. Integration must be intentional and supported by robust monitoring and evaluation from the outset to ensure it is sustained.
“Obesity is a long-term trend; you don’t have success in minutes, or even in years. You need at least 10 years of sustainability to see significant changes.”
Martine Laville, Professor Emeritus, Lyon 1 University, France
Imagine Jason again.
But this time, he lives in a world where obesity is taken seriously as a disease. As a result, its prevention and management is integrated into every day health promotion and health care services. He is included actively in his care plan, knows where to go and who to turn to. His care is connected between services and not scattered across them, and most potential complications are caught before they escalate. Jason no longer feels confused or blamed by the system. Instead, he feels supported, seen and in control of his health.
That is the kind of health care system people living with obesity deserve. And integrating obesity prevention and management into NCD care is one major step in that direction.






Audience key take aways
There is a need for all-of-society action on obesity–the solutions do not just lie in the healthcare system.
Position obesity at the heart of NCD prevention–progress on obesity unlocks progress across other major health targets.
A shift in narrative around health system funding to reflect the investment in keeping populations in good health rather than the cost of treating ill health.
We would like to thank the panellists and audience who took part in the discussion at The economic imperative: policy solutions for tackling non-communicable diseases, an Economist Impact event sponsored by Novo Nordisk on the sidelines of Abu Dhabi Global Health Week.
- Buthaina Abdulla Bin Belaila, Head of non-communicable diseases and mental health, Ministry of Health and Prevention, UAE
- Haleama Al Sabbah, Associate professor, Abu Dhabi University
- Sara Suliman, Clinical lead for obesity, genetics of diabetes and endocrinology, Imperial College London, Abu Dhabi
- Shereena Khamis Al Mazrouei, Director of health promotion and public health programmes, Abu Dhabi Public Health Centre
- Dan Beety, Senior director, global obesity policy and public affairs, Novo Nordisk
We will be continuing the conversation at upcoming events around the World Health Assembly and UN General Assembly, and welcome policymakers, advocates and changemakers to join us in advancing obesity on the global health agenda.
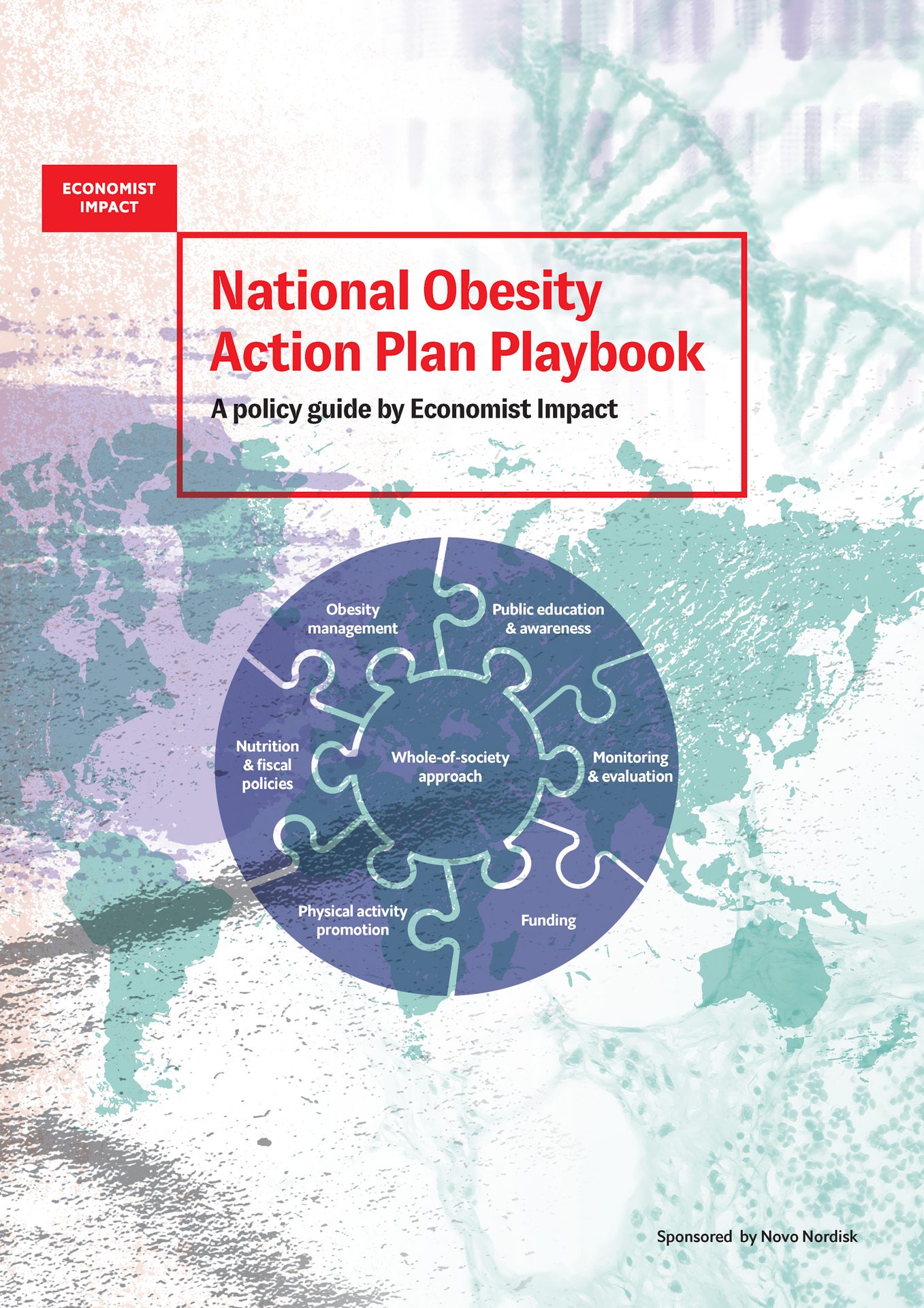
The National Obesity Action Plan Playbook contributes to advancing policy and national action on obesity by providing policymakers with a practical framework for designing and strengthening national strategies to prevent and manage obesity. Drawing on WHO guidance, global expertise, and case studies, it identifies key action areas and highlights best practices for tackling obesity’s systemic drivers through a whole-of-government and whole-of-society approach.
