National obesity
Action plan playbook
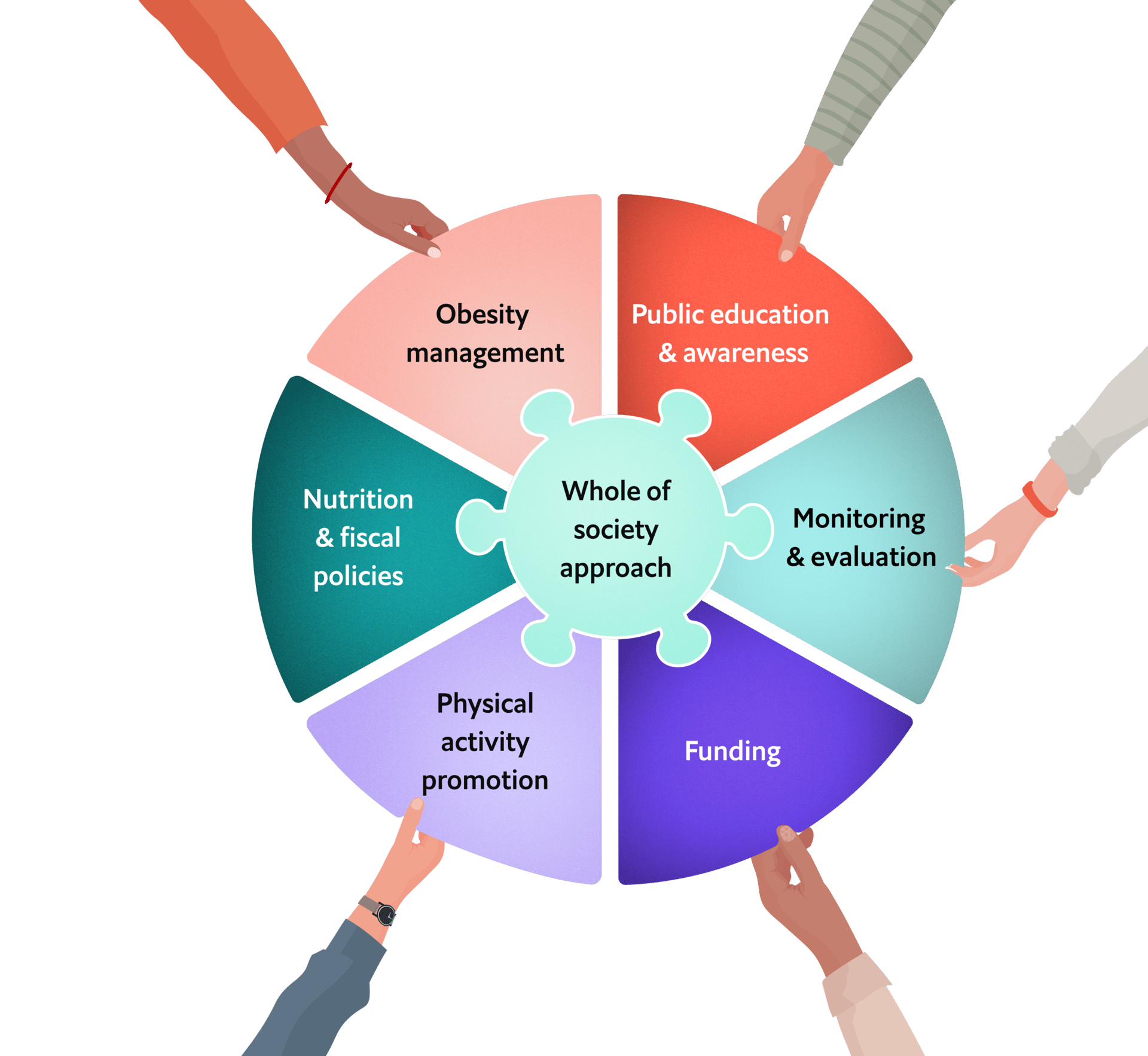
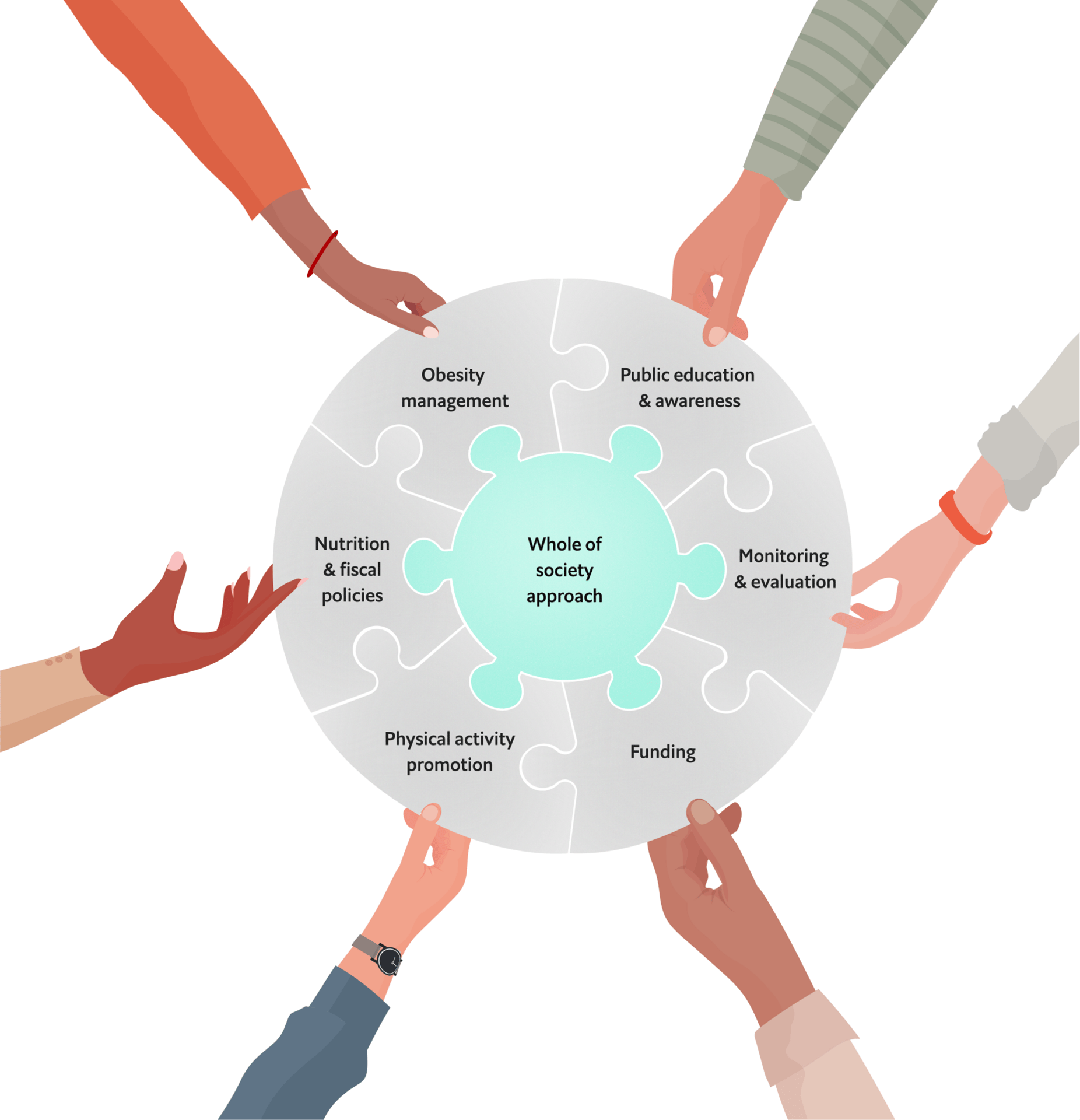
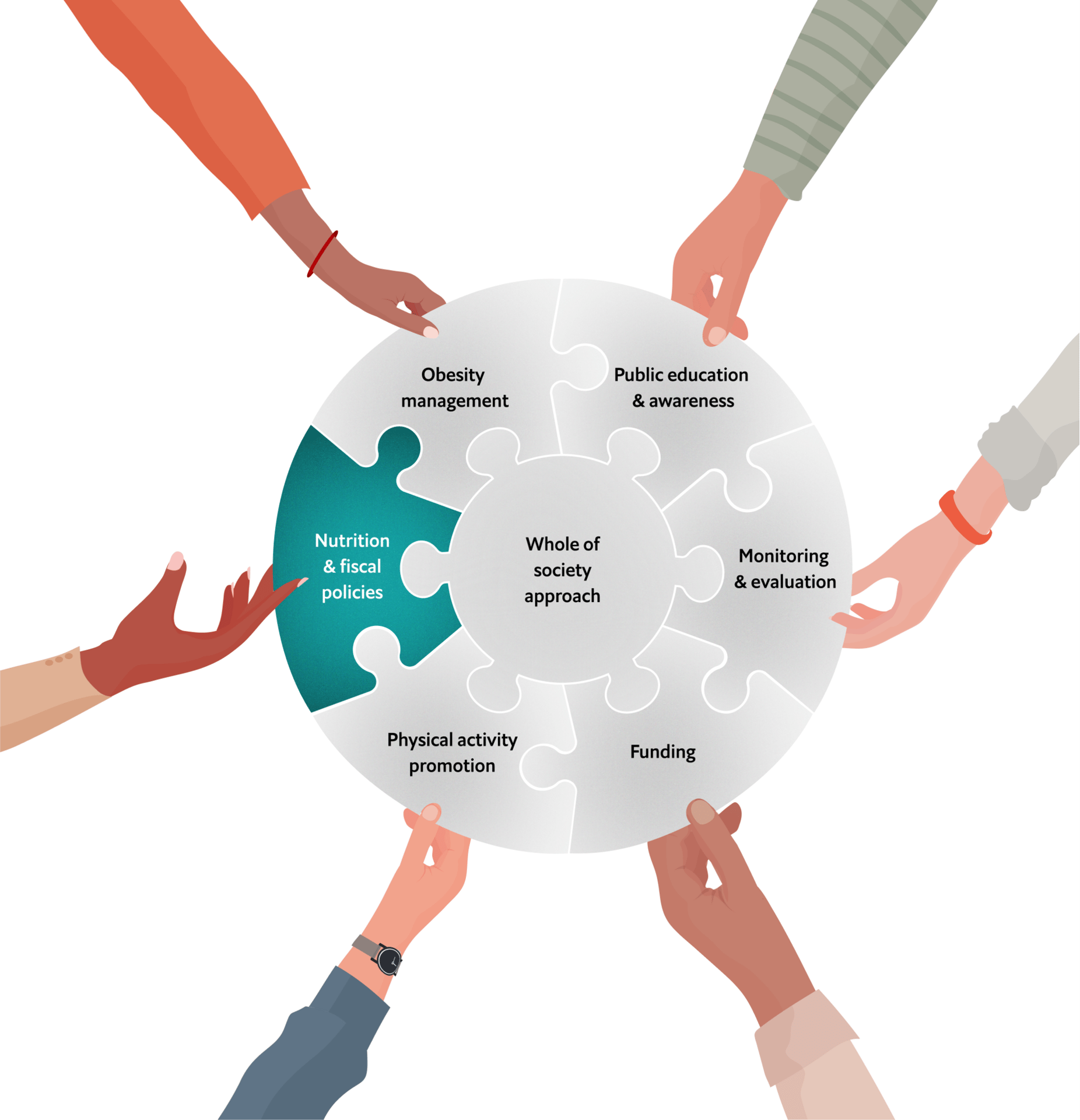
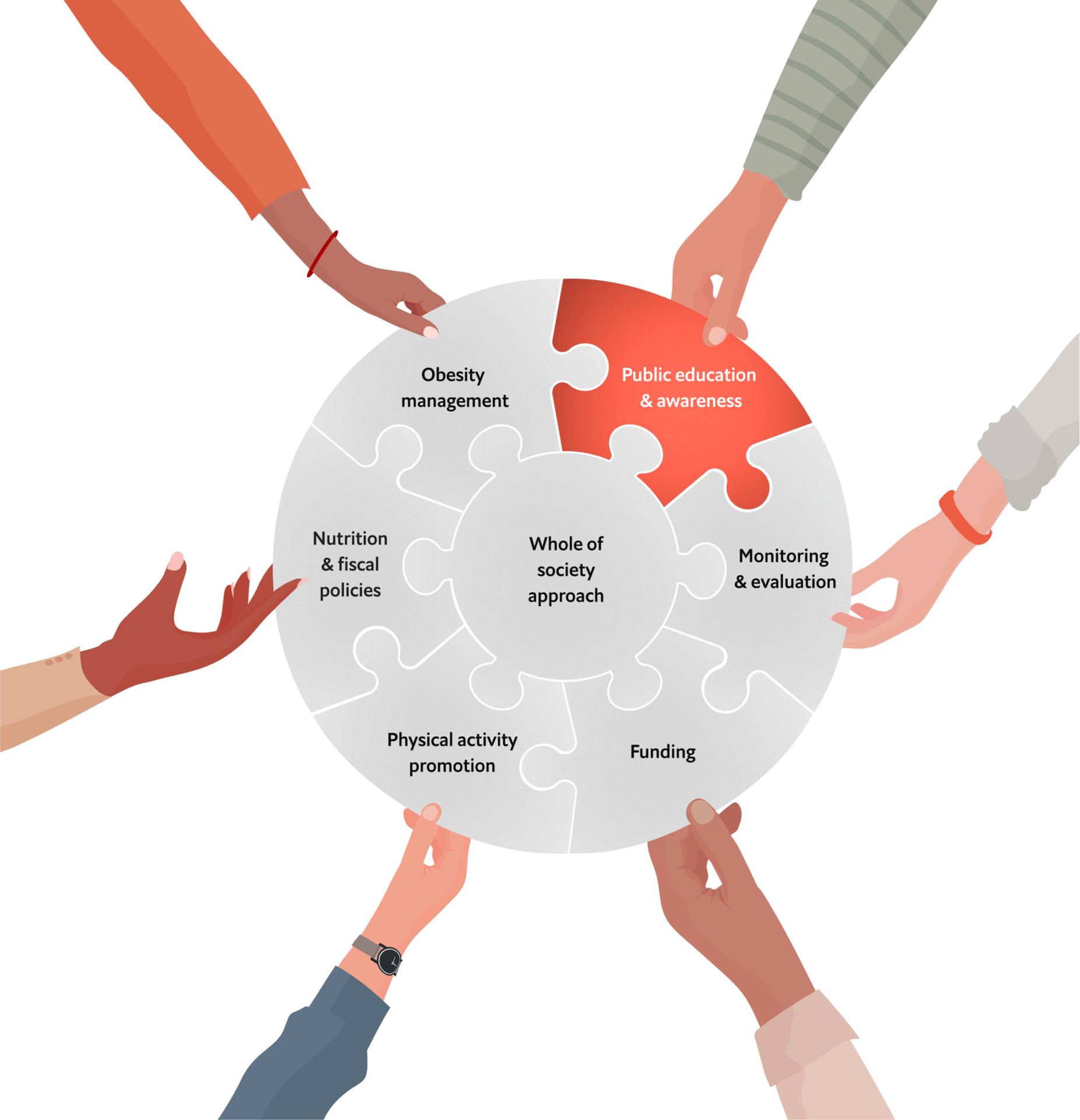
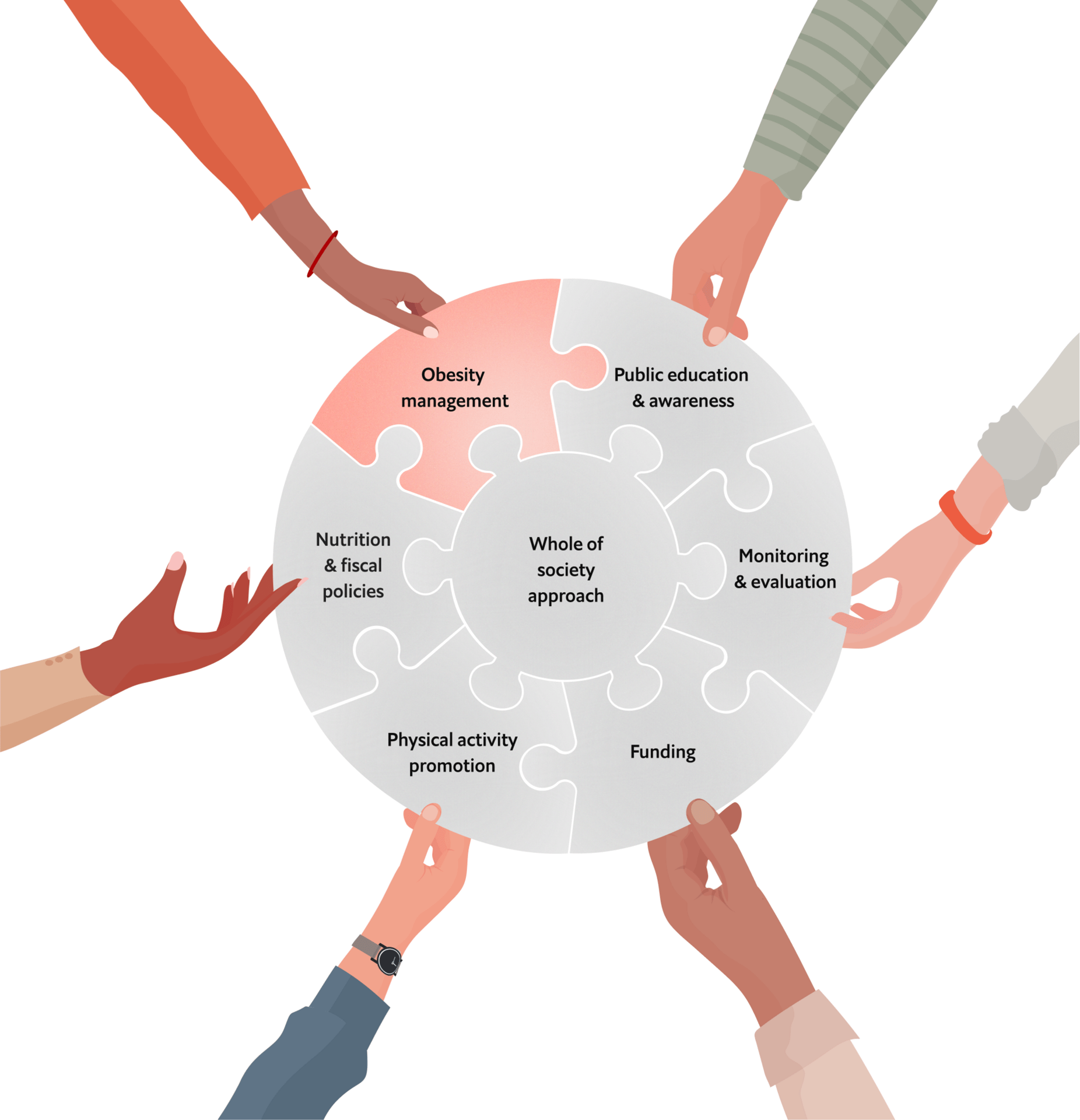
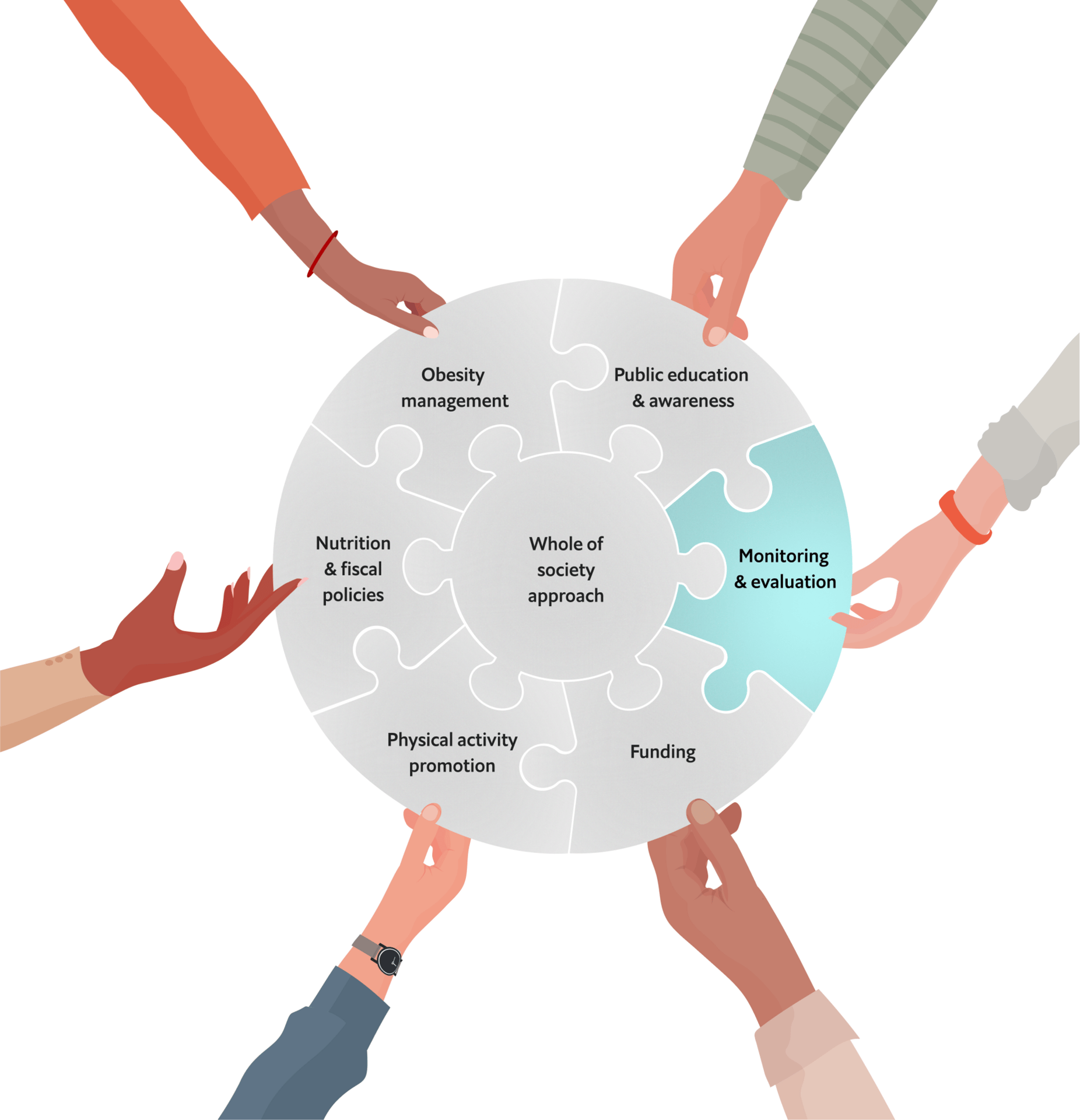
The National Obesity Action Plan Playbook contributes to advancing policy and national action on obesity by providing policymakers with a practical framework for designing and strengthening national strategies to prevent and manage obesity. Drawing on WHO guidance, global expertise, and case studies, it identifies key action areas and highlights best practices for tackling obesity’s systemic drivers through a whole-of-government and whole-of-society approach.
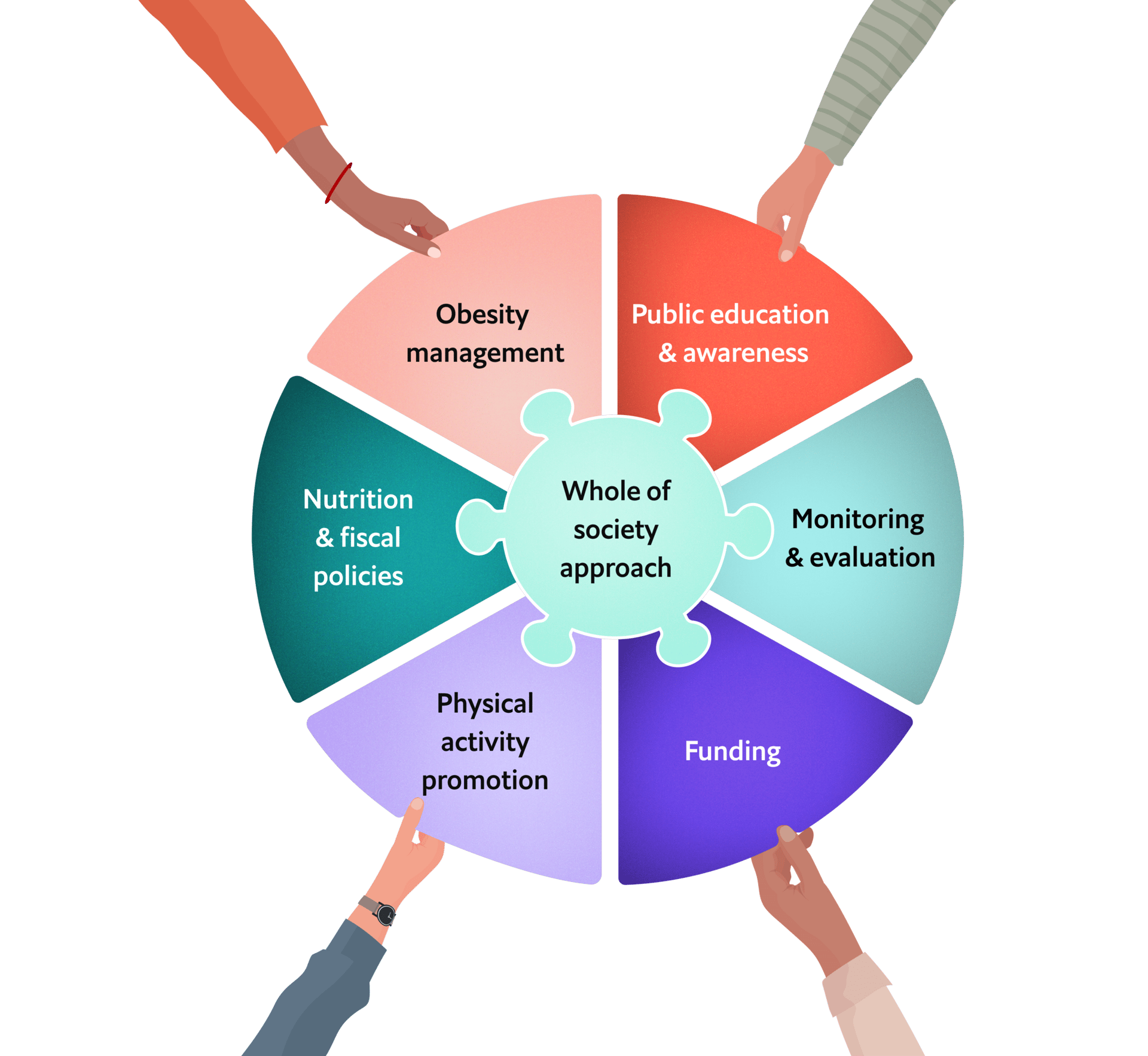
The National Obesity Action Plan Playbook contributes to advancing policy and national action on obesity by providing policymakers with a practical framework for designing and strengthening national strategies to prevent and manage obesity. Drawing on WHO guidance, global expertise, and case studies, it identifies key action areas and highlights best practices for tackling obesity’s systemic drivers through a whole-of-government and whole-of-society approach.

Best practice 1 – Spain implemented a structured classification system for government engagement. First, the national plan grouped all policies along “strategic lines”, or overarching goals. To bring clarity and focus, each policy under a strategic line was grouped according to the environment in which it would be implemented—for example, whether in education, the economy, or the digital sector. Within each of these environments, various government stakeholders were identified to play their part in advancing the policy.

Best practice 2 – Australia provided an example of strong implementation, applying a health-in-all-policies lens in areas such as urban planning, education, and economic planning, led by the Department of Health.
Why this matters
Obesity prevention and management is often fragmented and lacks inclusivity, failing to address the condition’s complex, multisectoral root causes effectively. As obesity is not only a health issue, but an economic and national development one as well, looking beyond health systems is necessary for effective mitigation efforts.
"We involved 15 ministries, 18 scientific societies, 13 civil society organisations, and 25 economic sector associations. The idea was to create a country plan—something everyone could align with"
Pedro Gullon, Spain
Key elements
Unifying collaboration: Addressing obesity demands a whole-of-society approach, detailing and assigning stakeholders’ responsibilities across government, academia, NGOs and the private sector to ensure accountability, efficiency and impact.
Integrating policy approaches: A “health-in-all-policies” approach embeds health considerations into policies across sectors, such as urban planning, education, and agriculture. This is essential to tackle the underlying social and environmental drivers of obesity, while also ensuring people living with obesity have access to quality care they need.
Components
- Whole-of-government approach:The following policies focus on implementing a whole-of-government approach aimed at fostering collaboration across various sectors and relevant government stakeholders to drive obesity policy forward.
- Ensuring health-in-all policies across sectors: Implement a health-in-all policies framework to ensure that health is considered across all sectors, addressing the various factors influencing obesity and promoting coordinated action at all levels of society.


Best practice
Here we highlight two examples of best practice, find more by downloading the playbook.
01
Whole-of-society approach
back to top
02
Nutrition and fiscal policies
Why this matters
Overweight and obesity are escalating globally, in part due to poor nutrition, unhealthy dietary practices, and inadequate early life interventions; this reality requires urgent action to ensure healthier diets, particularly for children and adolescents.
"We have been able to show that a sugar tax has decreased sugar intake or sugary beverage purchase, particularly amongst poorer people, which is really important because they often bear the brunt of the epidemic of obesity and diabetes."
Susan Goldstein, South Africa
Key elements
Improving access to healthy foods: Government subsidies and fiscal measures increase the affordability and availability of nutritious options, while curbing unhealthy options.
Enabling healthier options: Clear labelling, advertising regulations, and school-based interventions create environments that support healthier dietary behaviours across all age groups.
Addressing systemic barriers: Policies must tackle food affordability and security, while reducing health disparities to ensure equitable access to healthier diets.
Components
- Policies and programmes to enhance accessibility and affordability of healthy foods and beverages: Fiscal strategies, including financial investments, government programmes and community-driven approaches, improve both access to healthy foods and address the broader issue of food security.
- Fiscal policies to reduce access to unhealthy foods and beverages: Fiscal tools, such as taxes on sugar-sweetened beverages (SSBs) and unhealthy foods, aimed at reducing consumption and prompting positive changes in consumer behaviour.
- Nutrition labelling: Food-labelling as a key strategy to combat obesity, providing consumers with clear, easy-to-understand nutritional information that can guide healthier eating.
- Advertising and marketing of foods and beverages: Regulate marketing of unhealthy foods and beverages, especially to children, to reduce their attractiveness and encourage healthier eating habits.
- School-based nutrition policies: Increase the availability of nutritious foods and healthy drink options, such as water, to create an environment where school-aged children have easy access to healthier choices throughout the school day, while also establishing national nutritional standards to ensure the quality of food served at and around schools.


Best practice
Here we highlight five examples of best practice, find more by downloading the playbook.




Best practice 1 – Australia waives a Goods and Services Tax for certain foods, including fruits and vegetables and incorporates financial incentives to encourage the purchase and consumption of essential healthy foods like fruits, vegetables, and dairy.
Best practice 3 – Spain stands out by not only emphasising the need for improved labelling of processed foods to promote healthier eating, but also connecting this discussion to the broader food system. Specifically, it aligns with the European “Farm to Fork” strategy which aims to make food systems “fair, healthy, and environmentally-friendly.”
Best practice 4 – The UAE reinforced restrictions on advertising by taking a legal approach that reviews advertising legislation to evaluate its effectiveness and implementing strict enforcement mechanisms to ensure compliance.
Best practice 5 – Australia integrated healthy eating into school curricula and implemented zoning policies to reduce the number of fast-food outlets near schools.

Best practice 2 – Mexico's sugar-sweetened beverage tax reduces sugary drink consumption and increases water spending, while encouraging smaller portions and lower sugar, sodium, and fats in processed foods.
03
Physical activity
promotion
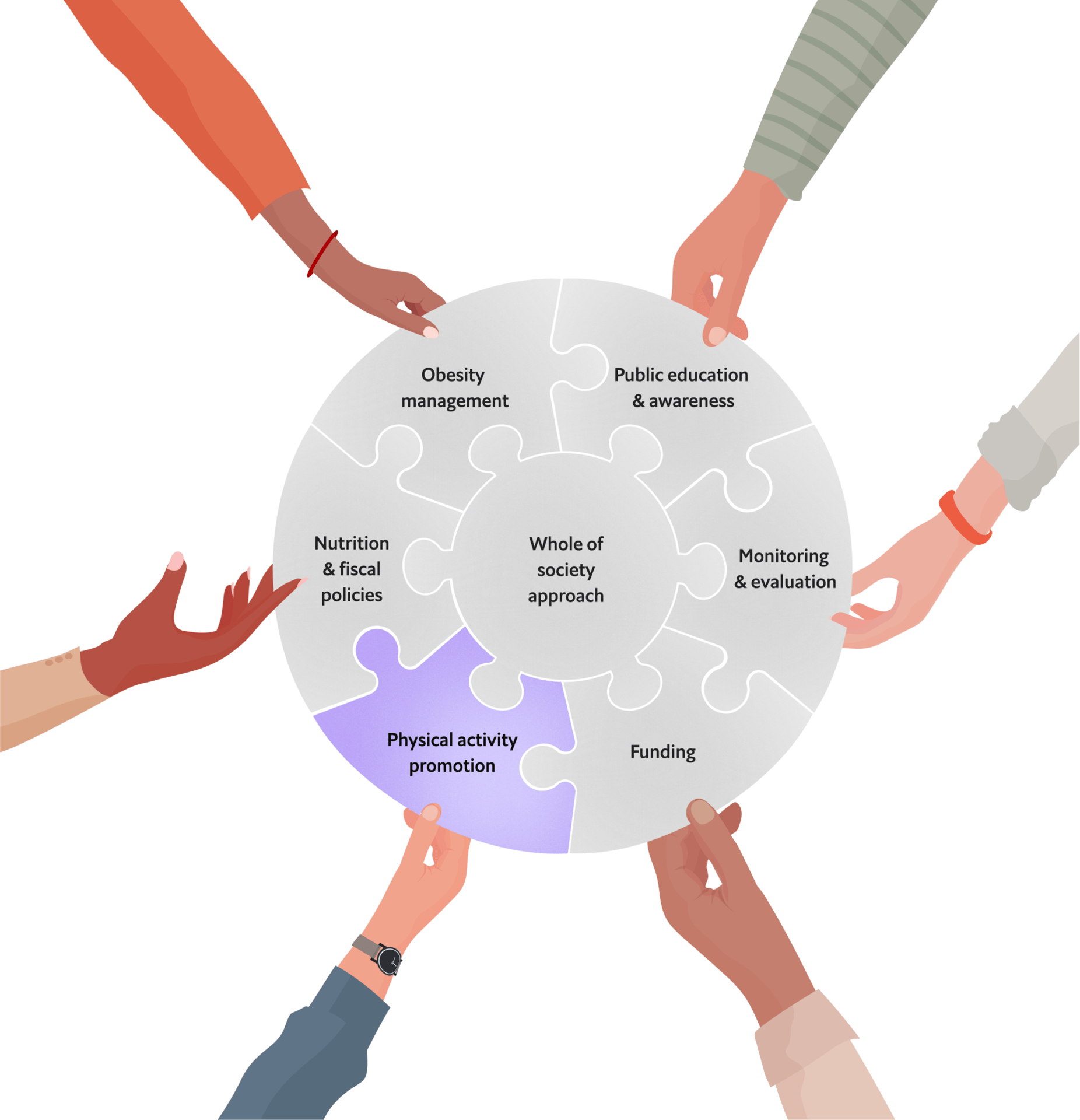
Why this matters
Globally, physical inactivity remains high, driven by urbanisation and unequal access to safe activity spaces. Worldwide, one in four adults, and three in four adolescents (aged 11–17 years), do not currently meet the recommendations for physical activity set by the WHO, which leads to significant health, social and economic costs.
"Active transport is a powerful public health tool because it cuts across health, air pollution, and climate change."
Alison Cox, Switzerland
Key elements
Changing urban design for daily activity: Effective physical activity policies embed movement into daily life through urban planning, active transport, and community programmes.
Engaging at school and community levels: Schools and community-based initiatives are critical in fostering lifelong physical activity habits, promoting inclusivity, and reducing barriers to participation.
Pairing nutrition and physical activity: Nutrition and physical activity must be addressed together as complementary strategies to prevent obesity and improve public health outcomes.
Components
- Guidelines on physical activity: Encourage national standards for physical activity as a key strategy to combat obesity, recognising that regular exercise is essential for maintaining a healthy weight and preventing obesity-related health issues.
- Infrastructure initiatives enabling physical activity: Support physical activity as a key way to combat obesity by expanding public transport and creating safe, accessible spaces for exercise, such as parks, walking paths, and recreational facilities.
- School-based physical activity policies: Encourage physical activity in schools as a strategy to combat obesity by integrating regular exercise into the school day and promoting active play.
- Community physical activity programmes: Encourage community-led programmes, tailored to address the unique needs and realities of local populations, which ultimately promote sustainable solutions for obesity prevention and management.


Best practice
Here we highlight four examples of best practice, find more by downloading the playbook.




Best practice 1 – Australia integrated its national physical activity guidelines into its national obesity plan, providing specific recommendations tailored to different age groups, while also linking physical activity initiatives to reduced screen time.
Best practice 3 – Spain implemented policies to adapt school spaces and facilities to meet the physical activity needs of all students, including “activating” these spaces for use outside of school hours and non-term periods.
Best practice 2 – Mexico focuses on diversifying public spaces for physical activity in cities like Mexico City, Puebla, and Guadalajara, such as through pedestrianising streets and building bike lanes.
Best practice 4 – South Africa has planned programmes like the Indigenous Games Festival and the National Golden Games promote physical activity while fostering inclusivity and celebrating cultural heritage.
04
Public education and awareness
Why this matters
The absence of effective campaigns on nutrition and physical activity limits health literacy, while inadequate understanding of obesity as a disease, combined with entrenched stigma, hinders efforts to empower individuals, tackle root causes, and foster supportive environments for obesity prevention and management.
"There are many excellent local initiatives, but they are scattered, small, and not sustainable. The future objective should be to gather all these efforts into a general plan while allowing local communities to organise and execute them effectively."
Martine Laville, France
Key elements
Creating healthier habits on nutrition: Integrating tailored nutrition education into schools, workplaces and healthcare supports the development of healthier eating habits.
Increasing physical activity campaigns at the local level to maintain active lifestyles: Launching local, community-driven initiatives and education campaigns promotes active lifestyles, reduces sedentary behaviours, and encourages long-lasting healthier habits for different groups in the population.
Dismantling weight stigma: Reducing weight stigma through targeted campaigns, inclusive policies, and medical workforce training could shift the conversation from personal responsibility to recognising obesity as a multifaceted disease. This approach not only alleviates bullying and discrimination, but also empowers individuals living with overweight or obesity to seek care and support without fear of judgment.
Components
- Nutrition education and counselling: Focus on providing nutrition education and counselling to help individuals make healthier food choices, prevent obesity, and manage weight-related issues, with the help of tools, such as nutrition-sensitive school curricula, digital platforms, family involvement and creative public outreach programmes.
- Cultivating active mindsets through awareness and daily practice: Implement physical activity campaigns to educate the public on the importance of regular exercise and combat obesity by promoting the maintenance of active lifestyles for various age groups.
- Reducing stigma and promoting inclusivity: Reduce discrimination, particularly in vulnerable populations, by shifting societal perceptions of obesity to recognise it as a multifaceted disease rather than solely a matter of personal responsibility.


Best practice
Here we highlight three examples of best practice, find more by downloading the playbook.



Best practice 1 – South Korea focused on targeted interventions across all ages, including puppet theatre for toddlers, "Planting Health Buds" for preschoolers, "Healthy Caring Playground" for older children, and public lectures for adults to promote healthy eating, physical activity, and obesity prevention.
Best practice 3 – Australia prioritised tackling weight stigma by implementing social marketing campaigns that used inclusive language and imagery. The plan also recognises the need to carefully test and evaluate social marketing and communications on their use of appropriate language, imagery and messages to avoid weight stigma and potential for adverse impacts while encouraging healthy eating and physical activity.
Best practice 2 – South Africa engaged local community leaders as role models to promote healthy lifestyles. These efforts focus on fostering grassroots-level engagement to ensure community ownership and sustainable impact on physical activity habits.
05
Obesity management
Why this matters
Many healthcare systems struggle to provide comprehensive obesity management due to limited access to multidisciplinary care, gaps in healthcare workforce training, and a lack of integration into routine health services. Addressing these issues will not only improve obesity management, but also streamline overall healthcare delivery.
“You can’t triple bypass your way out of an obesity epidemic.”
Amanda Lee, Australia
Key elements
Building healthcare workforce capacity: Expanding the healthcare workforce and resources for obesity prevention and management involves training a wide range of healthcare providers—including, but not limited to physicians, nutritionists, and psychologists—on obesity education and practical service delivery to ensure a holistic, patient-centred and multidisciplinary approach.
Integrating obesity into existing service delivery frameworks: Integrating services into existing chronic care pathways to provide comprehensive obesity care, including prevention, early diagnosis, screening for complications, treatment, rehabilitation, and long-term management to halt progression and reduce related health risks.
Improving access to universal health coverage for obesity care: Providing comprehensive and affordable preventive, curative and rehabilitative healthcare services guarantees that individuals can access the necessary care and support for treatment they need.
Components
- Healthcare workforce capacity-building: Build the capacity of healthcare professionals through training programmes, educational campaigns and upskilling to effectively address obesity using multi-disciplinary approaches.
- Personalised obesity management services: Personalise healthcare approaches to managing obesity, tailoring interventions to individual needs, lifestyle factors and health conditions, while also emphasising community-based support.
- Coordinated and integrated obesity management: Integrate obesity prevention and management into all levels of the healthcare system through coordinated, multi-disciplinary care models, which ensure that all individuals receive comprehensive, accessible, and personalised care throughout the life-course.
- Universal access to obesity care: Improving the access to, and affordability of, obesity care and ensuring that health services are culturally appropriate and timely, especially for under-served groups.


Best practice
Here we highlight four examples of best practice, find more by downloading the playbook.



Best practice 3 – The UAE has multi-professional teams deliver coordinated care for obesity management, aligned with existing clinical guidelines.
Best practice 1 – France focuses on workforce capacity training within its Centres Spécialisés de l’Obésité (Specialist Centres for Obesity), equipping healthcare professionals with multidisciplinary skills in nutrition, physiotherapy, and mental health, while prioritising professional development in therapeutic education, integrated care, and paediatric obesity management.
Best practice 2 – South Korea provides structured management plans for individuals with severe obesity, while also emphasising the importance of management around lifestyle factors such as stress, sleep, and alcohol use.
06
Monitoring and evaluation
Why this matters
Many countries lack robust monitoring and evaluation systems for obesity prevalence, related societal impacts of related policies, hindering their ability to track progress, tailor interventions, and adapt policies to the needs of diverse populations and emerging challenges.
“Without someone responsible for tracking progress, we had no idea which strategic objectives were met and which weren’t, so this time we wrote in specific responsibilities to ensure accountability and implementation.”
Jeanne Lubbe
Key elements
Disease surveillance: Leveraging national surveys, surveillance systems and electronic medical records to track obesity across subpopulations enables data-driven, targeted interventions and policy adjustments.
Evaluating policies for improvement: Integrated evaluation frameworks assess policy performance and ensure evidence-based improvements in obesity prevention and management.
Components
- Monitoring and surveillance of overweight and obesity: Monitor obesity prevalence, health status, risk factors and related impacts across different population groups, life stages and settings to better tailor interventions for diverse populations.
- Evaluation of obesity policies and programmes: Set ambitious outcomes and progress targets for obesity, and integrating evaluation systems to assess and refine policies and efforts, ensuring impact, guiding corrective actions, and informing future strategies.


Best practice
Here we highlight two examples of best practice, find more by downloading the playbook.

Best practice 1 – Australia consistently updates its National Child Measurement Programme, offering detailed insights into obesity trends by age, gender, and deprivation levels.

Best practice 2 – South Africa is notable for explicitly incorporating monitoring and evaluation at its plan's conception to ensure policies are effective and remain on-track.
07
Funding
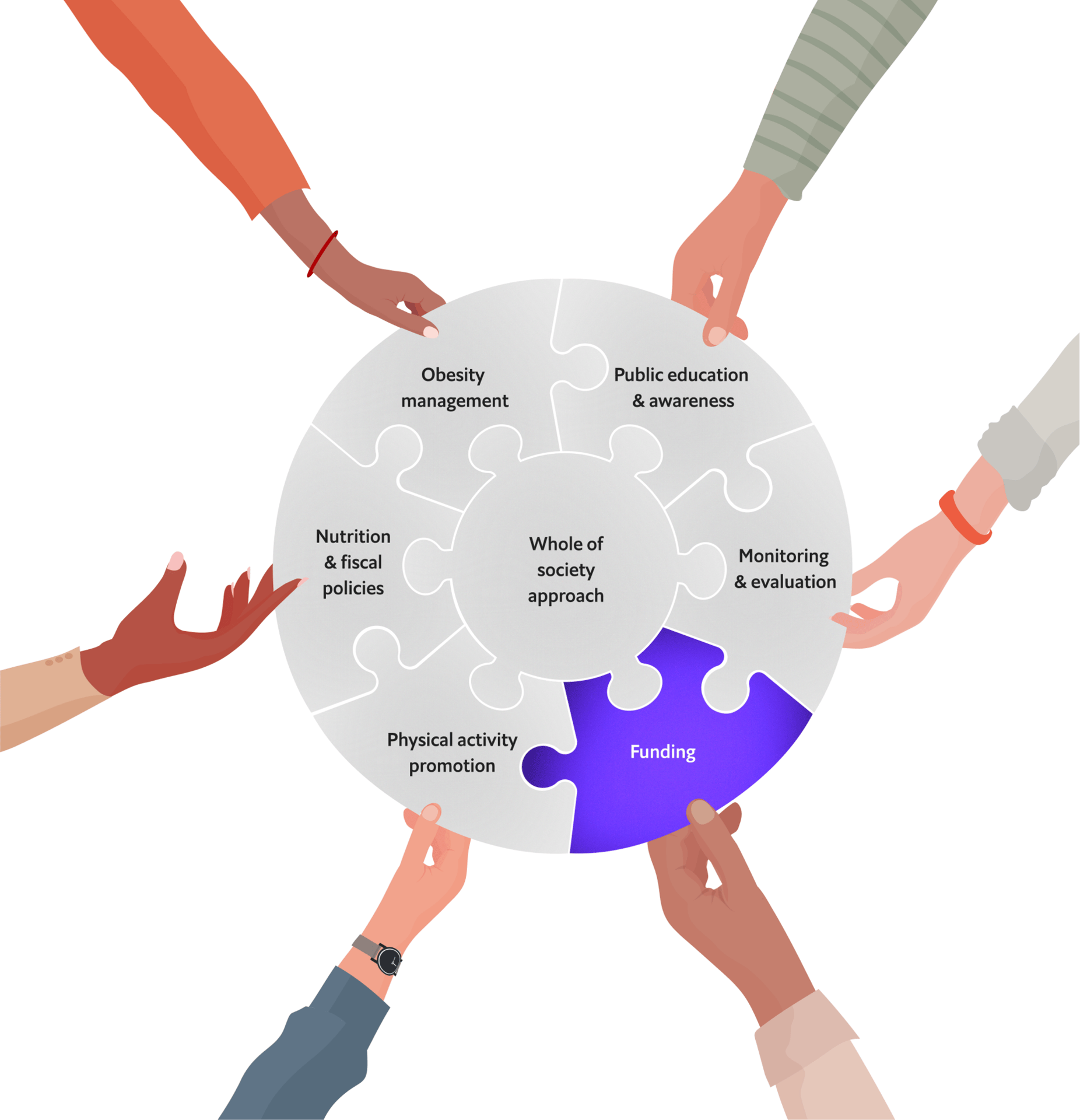
Why this matters
Many obesity prevention and management strategies lack sufficient and sustained funding, limiting their implementation and scalability. Transparent financial commitments and dedicated budgets are essential to ensure that policies are effective in the long term.
"Obesity is a long-term trend; you don’t have success in minutes, or even in years. You need at least 10 years of sustainability to see significant changes. But the problem is that a politician’s timeline is often just three months."
Martine Laville, France
Key elements
Establishing commitment and accountability through sustained funding: Long-term financial resources for monitoring and evaluation, as well as for prevention, health system strengthening, and universal coverage, demonstrates country commitment, enhances transparency, ensures accountability, and guarantees the effectiveness of obesity prevention policies.
Components
- Sustained funding for obesity prevention and management activities: Commitment to and allocation of earmarked, adequate, sustainable funding for obesity prevention and management efforts through national healthcare programs, including support for research, advocacy, and cross-sector collaboration.
- Funding for monitoring and evaluation: Outline resource needs, assigning responsibilities, and setting a monitoring plan for obesity prevention and management policies.


Best practice
Here we highlight two examples of best practice, find more by downloading the playbook.

Best practice 1 – Australia funds obesity management through its Medicare Benefit Scheme and National Health Reform Agreement, covering services like dietitians, psychologists, and exercise physiologists.

Best practice 2 – South Africa offers a well-defined breakdown of resource requirements for each policy measure in the mid- and end-term, ensuring transparency.
Article 01
What is obesity and why does it matter?
By 2035, around half of the world's population will be living with overweight or obesity, so a whole-of-government response is needed.

Article 02
Obesity: the role of genetics, biology and physiology
Our body's regulation of food intake is complex and very little of it is within our conscious control.
Article 03
Social determinants of health and obesity
Social determinants of health, including food marketing, built environment, education and income, contribute to the development of obesity.

Article 04
Mental health aspects of obesity
People living with obesity can face stigma, discrimination, low self-esteem and depression. Weight bias and stigma must not be tolerated.